An overview of Allergic Rhinitis
What is Allergic Rhinitis (Hay Fever)?
Allergic rhinitis (hay fever) is an allergic reaction to tiny particles in the air called allergens. When you breathe in allergens, your body reacts by releasing.. Despite being called hay fever, hay doesn’t cause hay fever and most people don’t get a fever.
Symptoms of hay fever include sneezing, nasal congestion and irritation of your nose, throat, mouth and eyes. Allergic rhinitis isn’t the same as infectious rhinitis, otherwise known as the common cold. Hay fever isn’t contagious. Also, not all rhinitis is allergic. Many people suffer from nonallergic rhinitis resulting in similar symptoms. Inflammation causes rhinitis, not allergens or histamine release.
When do people usually get hay fever?
You can have hay fever any time of the year. Seasonal allergies occur in the spring, summer and early fall when trees and weeds bloom and pollen counts are higher. But pollen seasons can vary depending on your location, as well. Perennial allergies can happen year-round. They result from irritants that are always around, such as pet dander, cockroaches and dust mites.
Causes of allergic rhinitis (hay fever)
Allergic rhinitis occurs when your body’s immune system reacts to an irritant in the air. The irritants (allergens) are so tiny that you can easily inhale them.
Allergens are harmless to most people. But if you have hay fever, your immune system thinks the allergen is intruding. Your immune system tries to protect your body by releasing natural chemicals into your bloodstream. The main chemical is called histamine. It causes mucous membranes in your nose, eyes and throat to become inflamed and itchy as they work to eject the allergen from your body.
Allergic rhinitis comes from many allergens, including:
1. Dust mites that live in carpets, drapes, bedding and furniture.
2. Pollen from trees, grass and weeds.
3. Pet dander (tiny flakes of dead skin cells).
4. Mold spores.
5. Cockroaches (their saliva and waste).
Food allergies can also cause inflammation in your nose and throat. Food allergies can be life-threatening, so get medical help right away if you’re concerned that a certain food is consistently causing allergy symptoms.
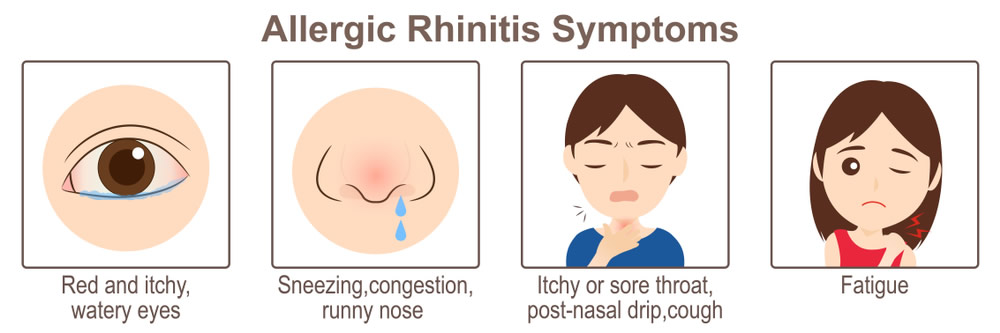
Signs and symptoms of allergic rhinitis (hay fever)
Hay fever symptoms can appear throughout the year. Outdoor allergies are worse in the spring, summer and early fall depending on where you live. In warm weather, weeds and flowers bloom, and pollen counts are higher. Indoor allergies, such as those from pets and dust mites, can get worse in winter because people spend more time indoors with their windows closed.
Symptoms of hay fever include:
1. Nasal stuffiness (congestion), sneezing and runny nose.
2. Itchy nose, throat and eyes.
3. Red or watery eyes.
4. Headaches, sinus pressure and dark circles under your eyes.
5. More mucus in your nose and throat.
6. Tiredness.
7. Sore throat from mucus dripping down your throat (postnasal drip).
8. Wheezing, coughing and trouble breathing.
Preventive measures against hay fever (allergic rhinitis)
There’s no way to prevent hay fever, but lifestyle changes can help you live with allergies. You can relieve hay fever symptoms by avoiding irritants as much as possible. To reduce symptoms, you should:
1. Avoid touching your face and rubbing your eyes or nose.
2. Close windows in your home and car during the spring, summer and early fall when pollen counts are higher.
3. Put covers on pillows, mattresses and box springs to protect against dust mites.
4. Keep pets off couches and beds, and close doors to bedrooms you don’t want them to enter.
5. Use filters in your vacuum cleaner and air conditioner to reduce the amount of allergens in the air.
6. Wash your hands often, especially after playing with pets.
7. Wear a hat and sunglasses to protect your eyes from pollen when you’re outside. Change your clothes as soon as you come indoors.
How Is hay fever (allergic rhinitis) Diagnosed?
As part of a normal vision screening, your child’s doctor will look for signs of amblyopia.
All kids ages 3 to 5 need to have their vision checked at least once.
Treatment for hay fever (allergic rhinitis)
Several allergy medications can improve symptoms and help you live with hay fever. These treatments come in many forms, including liquids, pills, eye drops, nasal sprays and injections. Talk to your provider before taking any medication, especially if you’re pregnant or have other health concerns.
Antihistamines
Antihistamine medications are available with a prescription or over the counter (OTC). They work by blocking the histamine that your body releases during an allergic response. Antihistamines come as pills, liquids, eye drops, nasal sprays and inhalers. They include:
1. Loratadine (Claritin®).
2. Cetirizine (Zyrtec®).
3. Fexofenadine (Allegra®).
4. Levocetirizine (Xyzal®).
Antihistamines can cause drowsiness. Avoid alcohol when taking antihistamines, especially if you’re going to drive.
Decongestants
These medications relieve congestion in your nose and sinuses. You can take decongestants by mouth (in pill or liquid form) or use a nasal spray. They include:
1. Afrin® nasal spray.
2. Phenylephrine nasal spray (Neo-Synephrine®).
3. Pseudoephedrine (Sudafed®).
Decongestants can increase blood pressure and cause headaches, trouble sleeping and irritability.
Nasal decongestants can be addictive when you use them for longer than five days.
Corticosteroid nasal sprays
These sprays and inhalers reduce inflammation and relieve symptoms of hay fever. The most common nasal sprays are Flonase®, Nasacort® and Rhinocort®. Side effects include headaches, nasal irritation, nosebleeds and cough.
Leukotriene inhibitors
During an allergic reaction, your body releases leukotrienes, histamine and other chemicals that cause inflammation and hay fever symptoms. Available only with a prescription, these pills block leukotriene. The most common leukotriene inhibitor is montelukast (Singulair®). Some people experience changes in mood, vivid dreams, involuntary muscle movements and skin rash when taking this medication.
Immunotherapy
This treatment works by helping your body learn to tolerate allergens. Your provider gives you a series of injections (allergy shots or subcutaneous immunotherapy) with a small amount of the allergen. Every time you get a shot, your provider increases the amount of the allergen. Over time, your immune system develops immunity to the allergen and stops launching a reaction to it.
In certain circumstances, your provider might recommend immunotherapy in the form of a pill that you place under your tongue called oral immunotherapy. Currently, oral immunotherapy is only available for allergies to trees, grass and dust mites (in the U.S.).
Complications
If you have allergic rhinitis, there's a risk you could develop further problems. A blocked or runny nose can result in difficulty sleeping, drowsiness during the daytime, irritability and problems concentrating. Allergic rhinitis can also make symptoms of asthma worse.
Frequently Asked Questions About hay fever (allergic rhinitis)
Hay fever is another name for allergic rhinitis. Hay fever mainly refers to seasonal allergic rhinitis, which is the allergies you experience at certain times of the year due to pollen from grass, weeds and trees. But some people use the terms interchangeably.
Seasonal allergies tend to occur in the spring and early fall when pollen from grass, trees and ragweed are more prevalent.
Seasonal allergies tend to happen at the same time each year. They often start suddenly and can last several weeks or until the allergen isn’t in the air anymore. Taking allergy medication to see if it improves your symptoms is one way to know if your symptoms are due to allergies. Checking a weather app or website to see if pollen is high in your area can also help you decide if what you feel is related to seasonal allergies.
People with airborne allergies have a higher risk of ear infections and sinus infections. Because hay fever can make it tough to get a good night’s sleep, you may feel tired during the day. If you have asthma, hay fever can make your asthma symptoms worse.